Our mission remains clear: to foster a collaborative environment that transcends competition, to reimagine the future of primary care. At the forefront of pivotal transformation, marked by the emergence of retail health, mergers and acquisitions and a broader shift towards value-based care, significant challenges such as patient access, engagement, and reimbursement persist. The Reimagining Primary Care Forum returns this year as a response to these challenges, recognizing the need to bring together key stakeholders and create actionable solutions to these shared challenges.
Are you seeking high-value connections and partnerships away from the crowds of larger conferences? Your search ends here. The Reimagining Primary Care Forum is an exclusive conference, capped at 100 attendees, providing a unique environment that brings together the most influential primary care visionaries in the space. Building on last year’s success, this year, we have created even more dedicated opportunities for you to make the most out of time, with an agenda filled with interactive sessions, action-focused roundtables and effortless group networking opportunities.
The Reimagining Primary Care Forum presents an enriching platform for learning and cross-sector collaboration across the entire primary care landscape. Bringing together the most prominent primary care stakeholders, from the likes of providers, health plan, retail health, academia and policy groups, and featuring the likes of: Cityblock Health, Humana, Corewell Health and Boston Medical Center, alongside emerging players such as Whole Foods Market and Amazon, this Forum offers you a place at the forefront of primary care innovation!
“Reimagining Primary Care isn’t just a slogan, it’s a necessity. I’m thrilled to share how Mirah’s collaborative care platform bridges the gap between physical and mental health, empowering primary care teams to deliver truly holistic care. Let’s build a future where mental health is not an afterthought but rather a fully participating member of a coordinated team.”
“I’m looking forward to learning from the leading voices in primary care from across the US.”
“I am excited to connect with primary care health professionals at the Reimagining Primary Care Forum to explore population-level analytics in primary care assessment. Innovations with “big data” can inform more effective public policy, facilitate improvements in equitable access to primary care, and promote higher performance for both systems and clinicians.”
“I am looking forward to connecting with professionals that are passionate about the direction and opportunities to reimagine primary care.”
“Coming together around primary care at this moment is crucial as we navigate the bedrock of value-based tactics for healthcare success.”
“My hope, as a rural subspecialist and rural health researcher, is to help develop ways to deliver better healthcare to rural America. This begins with conversations and with planning, and with this I am very excited to be able to meet and speak with new partners and colleagues in the 2024 Reimagining Primary Care Conference.”
“I look forward to collaborating with other thought leaders on strategies to foreground primary care in the U.S.”
“Data holds the key to unlocking a future where everyone receives tailored, effective primary care. I’m eager to join the conversation at Reimagining Primary Care about leveraging data insights to personalize care, address disparities, and ensure no one falls through the cracks. It’s time to make data work for patients, not just systems.”
2024 Speakers



Dr. Erica Savage-Jeter completed her undergraduate degree at Wofford College, Spartanburg, SC. Her training includes her medical degree from University of South Carolina School of Medicine, Family Medicine training at Palmetto Health Family Medicine Residency program and a master’s degree in business administration from Auburn University. Dr. Savage-Jeter started her medical career as a family physician in her hometown of Union, SC. Her practice became centered around the care of all age groups of people with preponderance of chronic illness including diabetes mellitus, congestive heart failure, atrial fibrillation, just to name a few. Dr. Savage-Jeter was also recognized for her commitment to provide evidence-based measures and excellent care to her patients with diabetes by the National Committee of Quality Assurance. In 2016, Dr. Savage-Jeter joined Partners in Primary Care, now CenterWell Senior Primary Care as it launched its care delivery model to Greenville SC. Her responsibilities during her tenure have grown from center medical director to Division Chief Medical Office. Her work has been focused on providing personalized healthcare with exceptional service to her personal patients as well as all the patients in her market with the goal to reduce the complexity and burden of disease and promote well-being while growing talent and developing physician leaders. CenterWell is committed to early disease detection, management of chronic diseases to prevent complications, and eliminating barriers to healthy lifestyle habits while nurturing a relationship of mutual trust and respect among all the patients and providers within CenterWell Senior Primary Care.



Dr. Lissy Hu serves as president of WellSky’s connected networks, where she works with leading health systems, payers, and accountable care organization to optimize post-acute care outcomes. Lissy brings with her over 15 years of experience working in the healthcare technology space. In 2012, Lissy founded CarePort to provide care coordination software solutions to manage patient transitions across the continuum. CarePort’s end-to-end platform bridge acute and post-acute EHRs – providing visibility for providers, payers, and ACOs into the care that patients receive across care settings. Lissy earned her Doctor of Medicine from Harvard Medical School. She holds a Master of Business Administration degree from the Harvard Business School and holds a Bachelor of Arts degree in pre-medical studies and sociology from Columbia University.



Mark Potter is the founder and CEO of Mirah, a behavioral health technology company. As a multi-industry veteran with extensive experience building high-performance teams, he has a passion for data and presenting it in a way that leads to actionable insights. It is this combination of experience and interest – along with marriage to a psychiatrist – that inspired the very founding of Mirah.
Before Mirah, Mark was the Senior Vice President of Global Operations for EnerNOC (now Enel X), where he grew the operations function from a team of one to over 400 people spanning five continents. He applies this same skill at Mirah today, having created a team of experts purpose-built to address the biggest challenges that stand in the way of successful behavioral health integration.






Aaron R. Hoffman, DO, MPH, is Medical Director and Assistant Professor for the Department of Physician Assistant Studies in the School of Health and Rehabilitation Sciences at MGH Institute of Health Professions. He is the Chief Clinical Innovation Engineer and a practicing family physician at Atrius Health in Boston, where he focuses on primary care for adults in an innovative, team-based practice.
His particular clinical interests include reproductive health, clinical education, and approaching primary care with a broad scope, including an array of procedures.
In addition to deep involvement in teaching IHP and Harvard Medical School students both clinically and in didactic sessions across several courses, Dr. Hoffman is also a faculty member at the Harvard Center for Primary Care, where he is co-director of the Harvard Home for Family Medicine.
Dr. Hoffman completed his undergraduate degree in Ancient Societies and Biology at Vassar College in Poughkeepsie, NY, and his Master’s in Public Health with a focus on health economics and policy at the Dartmouth Institute for Health Policy & Clinical Practice at Dartmouth College in Hanover, NH. He attended medical school at the Philadelphia College of Osteopathic Medicine, and completed his residency and chief residency in family medicine at Central Maine Medical Center in Lewiston, Maine.



Joel V. Brill, MD FACP is an executive clinician with over 35 years of experience providing strategic leadership and medical oversight to data-driven health organizations. He is skilled in strategy, development and implementation of innovative health programs, products and payment systems, with extensive experience in clinical practice, reimbursement, quality improvement, data analysis, and value-based care. Board Certified in Internal Medicine and Gastroenterology, Dr. Brill is an Assistant Clinical Professor of Medicine at the University of Arizona College of Medicine, and has been a CPT Advisor for over 25 years. Dr. Brill co-Chaired the Part D medication measures Technical Expert Panel for CMS, has published on episode and bundled payment methodologies, and developed and submitted advanced payment models to the HHS Physician Focused Payment Model Technical Advisory Committee. Dr. Brill received his undergraduate A.B. Biology at the University of California, Los Angeles, and graduated from the Rosalind Franklin University of Medicine and Science – Chicago Medical School. He completed his Internship and Residency in Internal Medicine at the UCLA – San Fernando Valley Program, a fellowship in Gastroenterology at Los Angeles County – USC Medical Center, and the Management Program for Health Care Organizations at the UCLA School of Public Health.



Nzinga Lowe is the Chief Executive Officer and Founder of Pygmalion Health, a healthcare advisory firm changing the narrative of healthcare by creating strategies that help providers prosper and patients thrive. She is an experienced global business advisor, value based care and clinical operations leader, health equity officer, and international speaker. She has traveled the world leading initiatives to: create opportunities for minority and women-led start-ups to gain funding, diversify portfolios of international VC firms, improve health outcomes for underserved populations, implement scalable value based care processes and initiatives, and increase performance for medical practices as well as large health systems. Nzinga has worked in the value based care space for many years, and has directly aided in the operational and financial success of many large-scale, national healthcare organizations. She is passionate about strategically improving the health outcomes of underserved populations and increasing their access to necessary resources and value based care. Her mission is to educate providers in value based care, conceptualize initiatives that improve their performance and processes, equip them with the framework to excel, as well as increase their revenue through lucrative partnerships and structured clinical workflows.



Kameron Leigh Matthews MD, JD, FAAFP is the Chief Health Officer of Cityblock Health, a transformative, value-based healthcare provider integrating medical, behavioral, and social services for Medicaid and dually eligible and low-income Medicare beneficiaries. A board-certified Family Physician, Dr. Matthews has focused her career on underserved and vulnerable communities, having held multiple leadership roles in correctional medicine, federally qualified health centers, and managed care. Most recently at the Veterans Health Administration, she led transformational efforts focused on integrated, Veteran-centered models of care including the implementation of the MISSION Act of 2018 and the EHR modernization effort. She is an elected member of the National Academy of Medicine. She is a member of the sixth class of the Aspen Institute’s Health Innovators Fellowship. She received her bachelor’s degree at Duke University, her medical degree at Johns Hopkins University, and her law degree at the University of Chicago. As a passion outside of work, she co-founded and co-direct the Tour for Diversity in Medicine, an initiative seeking to bring premedical enrichment activities to underrepresented minority high school and undergraduate students across the country.



Dr. Saria Saccocio is the Eastern Region Chief Medical Officer for Carelon Health. She brings 20+ years of clinical experience to our team. She has led award-winning quality programs, improving patient care across the continuum of health as a Chief Medical Officer for several health systems in the southeast. She received her Doctor of Medicine from the University of Florida, her Executive Master of Health Administration from the University of North Carolina-Chapel Hill, and completed her Family Medicine residency at the University of Miami before opening her own solo family practice. She continues to serve patients at the Greenville Free Medical Clinic.
Becker’s Hospital Review has recognized Dr. Saccocio as one of the top 100 Hospital and Health System CMOs to Know and has been elected to the Alpha Omega Alpha Medical Honor Society. Her extensive civic and community involvement has included serving with many organizations such as: the Modern Healthcare Women Advisory Board, board member for the Pisacano Leadership Foundation, South Carolina Hospital Association, United Way of Greenville County; Greenville Free Medical Clinic, Big Brothers Big Sisters of the Upstate, the South Carolina Academy of Family Physicians Board, and is an Alum of the Women’s Leadership Institute and the Diversity Leadership Institute at Furman University.



Dr. Erin McNeely is a general internal medicine physician and leader in primary care at Corewell Health West Michigan. Erin received her bachelor’s degree in biology at the University of Chicago and her medical degree at Loyola University Chicago. She completed residency and chief residency in internal medicine at Dartmouth Medical Center in New Hampshire.
Dr. McNeely’s current practice site is Corewell Health West Michigan’s high-risk Medicaid clinic on Sheldon Avenue in downtown Grand Rapids. She also serves as co-chair of the Corewell Health West Health Equity Expert Improvement Team.
She is a Corewell Health-Michigan State University Alliance grant recipient along with Dr. Richard Sadler, geographic epidemiology professor at Michigan State University, for health equity-focused study of Kent County built environment factors mapping to patient health conditions.
Erin’s other areas of clinical practice interest include cervical cancer, metabolic disease and hypertension, problems that disproportionately affect BIPOC (Black, Indigenous, People of Color) communities both locally and nationally.



Lara Terry brings her 20+ years of experience and expertise from working in large integrated healthcare systems, venture back healthcare companies, and academic medicine to Boston Medical Center Health System (BMCHS) where she serves as the Chief of Value Based Care. In this role, she addresses opportunities to improve clinical care delivery and risk based contractual performance using a data driven approach.
Prior to coming to BMCHS, Dr. Terry held leadership roles in large integrated healthcare systems including Atrius Health where she led Population Health and Mass General Brigham (MGB) where she led Medical Analytics and Informatics.
Before coming to MGB, Dr. Terry spent nearly a decade in healthcare start-ups including Kyruus and Dovetail Health. Dr. Terry spent the early years of her career in academic medicine at Harvard Medical School and Boston University School of Medicine where she served as Co-Director of the New England Centenarian Study and published over 20 peer-reviewed articles on correlates of healthy aging and longevity. Dr. Terry is an awardee of the Paul B. Beeson Physician Faculty Scholar in Aging, an honor awarded to national leaders in aging research.
Dr. Terry received her BS from Tufts University, her MPH at Harvard University and her MD from UMDNJ. She completed her residency in Internal Medicine, the Harvard Geriatrics Fellowship, and is board certified in both. Her current clinical practice involves caring for patients with symptoms of cognitive decline.




Dana McCalley is the VP of Value-Based Care at Navina, a physician-first AI platform that helps primary care organizations succeed in value-based care. She has 15+ years in healthcare with a focus on Quality Improvement, Risk Adjustment, and Population Health. For more than a decade, Dana led one of the nation’s top performing ACOs, where she was responsible for helping 700+ clinicians provide care to 230k value-based patients. Her efforts led to over $159 million dollars in CMS ACO Shared Savings throughout her tenure. Dana received her Bachelors of Psychology from the University of South Florida and her Masters of Business Administration from Liberty University.



Dr. Megan Mahoney is the Hellman Professor and Chair of Family and Community Medicine at University of California San Francisco. Her career has been dedicated to transforming health systems and advancing population-based care. As Chief of Primary Care from 2015 to 2022, Dr. Mahoney led a dynamic team in implementing Primary Care 2.0, delivering fully integrated care with a digital first, team-based approach. Serving as President of the Medical Staff from 2020 to 2022, she oversaw transformative initiatives for physician well-being, health equity, and diversity at Stanford Medicine. In her current role as Chair of Family and Community Medicine at UCSF, she leads a department with a recognized legacy for primary care transformation in the social justice movement. Dr. Mahoney’s national influence is evident in her service on boards like The Doctors Company and the Editorial Board for the Journal of the American Board of Family Medicine. Her vision for inclusive and equitable primary care evolves to meet the dynamic needs of patients and communities.



Dr. Katherine Gergen Barnett is the Vice Chair of Primary Care Innovation and Transformation in the Department of Family Medicine at Boston Medical Center (BMC), a Clinical Associate Professor at Boston University Chobanian & Avedisian School of Medicine, an Associate at Harvard’s Center for Primary Care, and a Health Innovators Fellow at the Aspen Institute, a highly competitive fellowship that catalyzes leaders to improve US health care.
Prior to joining BMC in 2009, Dr. Gergen Barnett attended Yale University School of Medicine, worked at the National Institutes of Health, and completed a fellowship studying a model of group prenatal care for women in low-income communities. At BMC, she has served in multiple leadership roles including as a chief resident, Director of Integrative Medicine, Medical Director, Residency Director, and Vice Chair. Her primary clinical interests are behavioral health, preventive medicine, nutrition, trauma informed care, gender affirming care, women’s health, reproductive care, mindfulness-based stress reduction, and group medical care.
Dr. Gergen Barnett’s research career has been focused on innovative models of care to address chronic medical conditions, physician burnout, and engaging community partners in creating feasible solutions to increase health and wellness and to address medical distrust in traditionally marginalized communities. Dr. Gergen Barnett brings her training and passion for community engaged research to her role as PI in a clinical trial evaluating the safety and efficacy of Paxlovid, an antiviral, in treating high risk children infected with COVID-19.
Finally, Dr. Gergen Barnett is involved in local and state health policy addressing health inequities, national policy addressing primary care delivery, and is a regular contributor to The Boston Globe, Boston Public Radio, and multiple television outlets.



Dr. Chou serves as the Sr. Medical Director of Medical Management at Oak Street Health, a network of value-based primary care centers for adults on Medicare. Dr. Chou supports over 600 providers and their care teams across over 200 centers in 25-plus states in the prevention of avoidable hospital admissions and readmissions. This role entails strategizing care delivery for the nation’s most at-risk patients in underserved communities and implementing the strategies at scale. She also serves as a primary care provider in Arizona.



Gary Price is a Board Member and the current President of The Physicians Foundation. As a board-certified plastic surgeon, he has served as an attending surgeon and clinical assistant professor of surgery at Yale-New Haven Hospital. Additionally, he is affiliated with numerous local and national medical associations and societies and is a past President of the Connecticut State Medical Society and the Connecticut and New England Societies of Plastic and Reconstructive Surgeons. He received his M.D. from the Pennsylvania State University College of Medicine and completed residency training in Surgery and Plastic Surgery at Yale. Dr. Price holds an MBA from the Yale School of Management. Under his leadership, the Physicians Foundation has successfully supported surveys, grants, research, public awareness campaigns and leadership training regarding physician wellness.
Dr. Price is a subject matter expert on topics including physician burnout, social drivers of health, issues facing physician practices, physician wellbeing and leadership. He has been featured in numerous publications including The New York Times, The Washington Post, Kaiser Health News, The Wall Street Journal, Politico, NBC News and Radio, Health Leaders, MedPage Today, Modern Healthcare and Medscape. Having addressed national and international audiences on physician wellness issues for many years, Dr. Price is a staunch advocate of practical steps towards systemic change aimed at reducing burnout in our health care workforce.



Jessica Lyons is a Licensed Marriage and Family Therapist with two decades of clinical practice experience. An Adjunct Professor at the University of New Hampshire, she is also co-founder of Aloft Integrated Wellness, LLC. Aloft, which was nominated for the 2023 National Small Business of The Year Innovation award, successfully implemented one of the first pediatric and adolescent collaborative care programs in the country.
A frequent presenter, Jessica is a nationally recognized expert in the Collaborative Care Model (CoCM) and mental healthcare innovation. She is a Clinical Advisor to Mirah.



Laura Fox, MPH is the Director of Payment Innovation for Blue Shield of California. In her role on the Provider Performance, Quality, and Affordability team Laura leads a team to design, build, test, and scale innovative ways to appropriately reward and incentivize providers to deliver care that is “worthy of our family and friends and is sustainably affordable.” The Payment Innovation team has designed and launched over 18 value-based payment models for primary care and specialty care services that are scaling throughout the state of California.
Laura is coming up on her 8-year anniversary with Blue Shield of California. Prior to her current role at Blue Shield as the Director of Chronic Disease Prevention for the Baltimore City Health Department leading programs aimed at improving health outcomes for Baltimore City residents.
Laura holds a master’s in public health From Johns Hopkins University and a Bachelor of Science degree in Biology from Brandeis University.



Dr. Lisa Rotenstein is a primary care physician (PCP), researcher, and operational leader. She is an Assistant Professor of Medicine, Medical Director of Ambulatory Quality and Safety, and Primary Care Physician at UCSF Health. She additionally serves as the Director of the Physicians Foundation and Brigham and Women’s Hospital Center for Physician Experience and Practice Excellence. Previously, she served as an Assistant Professor of Medicine and Medical Director of Population Health at Brigham and Women’s Hospital, where she oversaw ambulatory quality and integrated behavioral health for BWH’s 150,000+ patients across sixteen practices.
Dr. Rotenstein’s research focuses on enhancing outpatient care delivery, the clinician experience, and the intersection of the electronic health record with these issues. Her research and writing have been published in JAMA, JAMA Internal Medicine, The New England Journal of Medicine, The Harvard Business Review, and more. She has presented her work to the National Academy of Medicine, Department of Health and Human Services leadership, and the Office of the Surgeon General.
Dr. Rotenstein was named a 2021 STAT Wunderkind, a 2022 Modern Healthcare Top 25 Emerging Leader, and the 2022 Society of General Internal Medicine New England Region Investigator of the Year.






Eyal Kedar, MD is the Medical Director of Clinical and Rural Health Research at St. Lawrence Health in New York. As the sole rheumatologist for a large rural area in the North Country region of New York, he developed a connective tissue disease-associated interstitial lung disease (CTD-ILD) clinic to meet the needs of his patients. His combined rheumatology/ILD skillset has enabled him to continue to serve as one of the members of St. Lawrence Health’s inpatient COVID-19 treatment team. He is a member of the ACTIV-1 writing team and is a regular contributor to The Daily Yonder. His work and research are focused on the delivery of complex and rare disease care in rural areas.
St. Lawrence Health’s Department of Clinical and Rural Health Research was the recipient of the New York State Association for Rural Health’s Outstanding Rural Health Program of the Year in 2022.



Steve Holloway is an experienced public health professional, professor, and board member serving organizations with a public and community health focus. He is currently serving as the Director of the Health Access Branch at the Colorado Department of Public Health and Environment, a position he has held since October 2011. Additionally, he is an Adjunct Professor at the Graduate School of Social Work at the University of Denver, where he teaches courses on mental health and substance use policy, social determinants of health, and public policy.
Steve has a Master of Public Health from Emory University, a Graduate Certificate in Maternal and Child Health from the University of Arizona, and a Bachelor of Science in Biology from the University of Colorado. He has also completed several fellowships in health policy, informatics and leadership including the Advanced Leadership Training Program of the Regional Institute for Health and Environmental Leadership.
In addition to his professional and academic roles, Holloway serves on several boards and commissions, including the Health Workforce Cabinet of Governor Polis, the Rural Provider Access and Affordability Stimulus Advisory Committee, the Colorado Primary Care Collaborative, the Institutional Review Board for Human Subjects Research at the health department, and he formally served by appointment of the US Secretary on Health and Human Services on a commission for the analysis of the health professional workforce. Steve is also the Chairman of the Board at the Sewall Child Development Center in Denver, a member of the Master of Health Administration Advisory Board at the Metropolitan State University of Denver, and an advisor to the Center for Health Workforce Studies at the State University of New York.
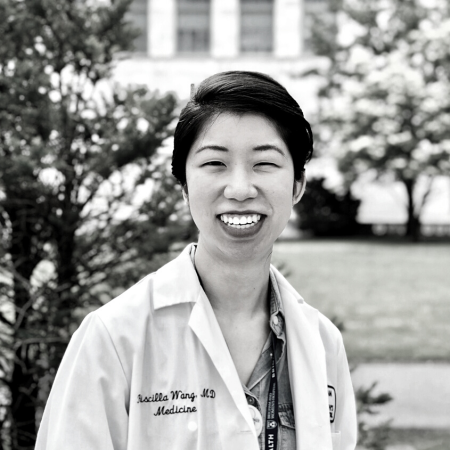


Priscilla Wang, MD MPH is a primary care physician at Massachusetts General Hospital and Associate Medical Director for Primary Care Health Equity at Mass General Brigham (MGB) in the Office of the Chief Medical Officer, leading system efforts to close clinical disparities via its United Against Racism campaign. Her work seeks to address inequities in health care, via structural interventions (particularly complex care interventions) that target systemic drivers of health disparities. She has previously served as Clinical Lead for MGB’s Medicaid ACO Community Partners and ED Navigator programs supporting vulnerable and complex patient populations, cofounded national patient advocacy campaigns to promote access to health care, and advised health policy work in the U.S. Office of Health Reform and the U.S. Office of the Surgeon General. She completed her MD at the Yale School of Medicine, MPH at the Harvard School of Public Health, and residency and fellowship training at Mass General Brigham.
Partner with Us
Bringing together senior-level executives from across the industry, the Reimagining Primary Care Forum promises an unrivalled networking and learning opportunity for everyone working in this space.
This forum provides a rare opportunity to showcase your offering to a dedicated, world-class audience. Spaces are limited this year!
Please contact our Commercial Manager Elliott (elliott@greygreenmedia.com), to discuss opportunities for involvement.


Location
The Reimagining Primary Care Forum 2024 will be taking place in Boston, MA. Stay tuned for more information – or email bethany@greygreenmedia.com to be the first to know!
2024 Partners


Carelon Health is an integrated care delivery system that harnesses the power of teamwork to address whole-health needs. Focusing on prevention and highly coordinated care, its innovative clinical model and value-based approach to managing complex chronic disease proactively addresses the physical, behavioral, and social drivers of its patients. Recognized for clinical outcomes above the national average, Carelon Health has expanded to 14 states as well as the District of Columbia, and serves over 100,000 Medicare Advantage and Medicaid patients. To learn more, go to www.carelonhealth.com and follow us on Twitter, LinkedIn, YouTube and Facebook @carelonhealth.


Hello Heart is the digital leader in preventive heart health. We provide members with a connected device and AI-driven digital coaching app. Through human-centric design, members receive actionable insights around healthy eating, activity, and can track key heart metrics like blood pressure and cholesterol unique to each person and consistent with clinical guidelines. By building a habit of monitoring heart health, members create sustained lifestyle changes. Validated in peer-reviewed studies, Hello Heart members achieve significant reductions in blood pressure over a sustained period. Founded in 2013, Hello Heart is a member of the American Heart Association’s Innovators’ Network and trusted by leading Fortune 1000 employers, national health plans and pharmacy benefit managers. Visit www.helloheart.com for more information.


Mirah is revolutionizing behavioral healthcare by bridging the gap between data and action. Beyond simply measuring progress, Mirah helps foster a collaborative care ecosystem where providers, patients, and communities work hand-in-hand. Our robust platform empowers data-driven decision-making, drives patient engagement, and unlocks the power of analytics to prove and improve behavioral health outcomes. Sustainable change, however, demands more than tech. That’s why partnering with Mirah includes custom implementation plans and ongoing support for collaborative care. This approach empowers organizations of all sizes to advance effective, integrated behavioral healthcare – ensuring positive change for both individuals and populations.


WellSky is one of America’s largest and most innovative healthcare technology companies leading the movement for intelligent, coordinated care. Our solutions seamlessly integrate acute and post-acute EHR data, offering comprehensive insights into the entire patient journey for providers, physicians, payers, and ACOs. These solutions empower healthcare professionals to streamline and enhance the coordination of patient care, enabling them to closely monitor and manage patients as they progress through the continuum.
Navina is a primary-care focused AI platform that transforms fragmented patient data into actionable insights at the point of care, reducing physician burden and improving value-based outcomes. Navina uses medically informed AI to read and interpret complex data from EHRs, HIE, labs, discharge notes, imaging results, claims, and more to create a concise, complete, and timely patient health profile, allowing clinicians to assess and act on their patient’s health status in the moment of care. Privia Health, Tampa General Hospital, and Millennium Physician Group are among some of the leading value-based organizations leveraging Navina’s AI platform to transform primary care. The company was named to the CB Insights AI 100 list of most innovative artificial intelligence companies in the world for 2023 and the Digital Health 50 list.
iRhythm is a leading digital healthcare company that creates trusted solutions that detect, predict, and prevent disease. Through a relentless focus on patient care, our vision is to deliver better data, better insights, and better health for all. We’re on a mission to address the future of healthcare, partnering with value-based organizations to detect and prevent cardiovascular disease – all while helping you save money and save lives. Through the Zio service, we aim to improve patient access and point of care diagnostics to enable optimized care coordination and quality outcomes through earlier detection of cardiac arrhythmias. Our goal is to keep appropriate patients with their primary care provider, while closing specialty care gaps that can lead to unnecessary healthcare resource utilization. In an era where the focus is on delivering better patient outcomes and more cost-effective care, iRhythm emerges as the partner of choice. We invite you to join us in this journey toward a healthier tomorrow, where every heartbeat matters and every patient has the chance to live a fuller, healthier life.


Wellinks excels in partnering with value-based primary care teams to manage COPD and chronic conditions through a specialized approach. Our model integrates virtual pulmonary rehab and tailored clinical coaching, enhancing self-management and overall well-being. Recognized by leading healthcare teams, Wellinks commits to elevating care quality and cost-efficiency, backed by a unique pay-for-performance guarantee. This assurance reflects our confidence in delivering measurable improvements in patient health outcomes, aligning with the goals of innovative care providers. For more information, visit wellinks.com
The Business of Primary Care is a media company created to support, encourage and educate primary care leaders and their teams.
Register for the Event
For pricing and booking options please click the button to go to the registration page.
